Introduction
In conflict-affected regions, the scars of war, displacement, and trauma run deep. Psychological wounds often remain long after the fighting stops, affecting individuals, families, and entire communities. According to the World Health Organization (WHO), one in five people in conflict zones experience mental health conditions such as depression, anxiety, or post-traumatic stress disorder (PTSD). However, access to mental health care remains scarce, leaving many to suffer in silence.
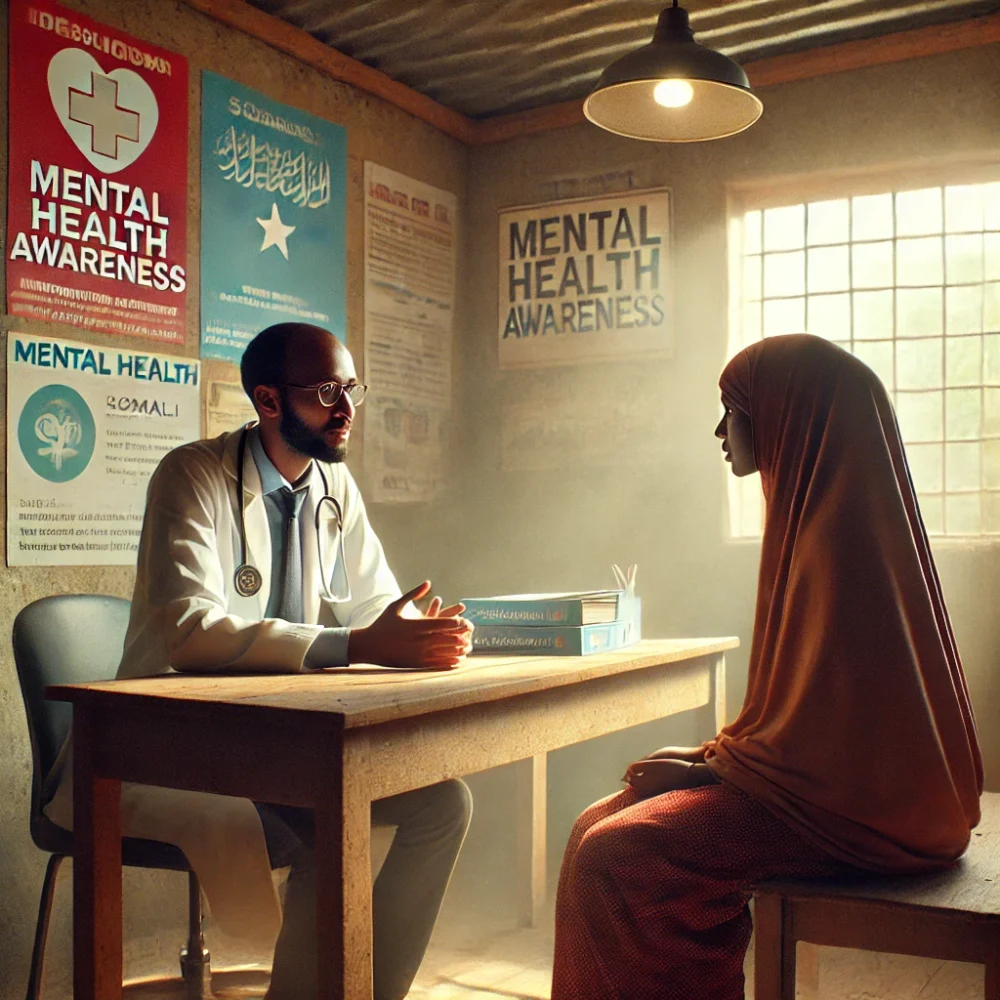
This case study explores how a community-led group therapy initiative helped survivors in a war-torn region find healing, connection, and hope. By providing safe spaces for collective healing, group therapy not only improved individual mental well-being but also strengthened community resilience.
The Challenge: A Community in Psychological Crisis
Before the introduction of group therapy, the conflict-affected community faced significant mental health challenges:
-
High levels of trauma and PTSD: A survey conducted by a humanitarian organization found that 65% of residents exhibited symptoms of PTSD.
-
Widespread depression and anxiety: Due to the loss of loved ones, homes, and livelihoods, 50% of community members reported feelings of extreme sadness and hopelessness.
-
Limited access to mental health care: With no trained therapists in the area, people had nowhere to seek professional help.
-
Social isolation and stigma: Mental health issues were heavily stigmatized, leading many to suffer in silence rather than seek support.
Realizing the urgent need for mental health intervention, a team of humanitarian workers, psychologists, and community leaders collaborated to implement group therapy sessions as a cost-effective and culturally appropriate solution.
The Solution: Implementing Community-Led Group Therapy
1. Training Community Leaders as Facilitators
Since professional mental health care was limited, the initiative focused on training trusted community members to lead group therapy sessions.
✔️ 30 community leaders and volunteers underwent mental health first aid and trauma counseling training.
✔️ Facilitators were equipped with techniques for active listening, guided discussion, and emotional support.
✔️ Religious leaders and elders were engaged to help reduce stigma and encourage participation.
Result: Within six months, over 200 individuals joined the therapy groups, demonstrating a growing trust in the program.
2. Creating Safe Spaces for Shared Healing
To make therapy accessible, group sessions were held in familiar, safe community spaces such as local schools, mosques, and women’s centers.
📌 Separate groups were created for different demographics, including women, men, and youth, to ensure comfort and openness.
📌 Confidentiality and respect were emphasized to build trust among participants.
📌 Sessions incorporated storytelling, art therapy, and role-playing to help participants express their emotions.
Result: Participants reported feeling 40% less isolated and found strength in shared experiences and mutual support.
3. Addressing Trauma Through Structured Therapy Sessions
The group therapy model followed a 12-week guided program tailored to trauma recovery.
🧠 Phase 1 – Understanding Trauma: Educating participants about PTSD, anxiety, and emotional healing.
❤️ Phase 2 – Emotional Expression: Encouraging participants to share their experiences and emotions in a safe space.
💪 Phase 3 – Coping Strategies: Teaching stress management techniques, mindfulness, and relaxation exercises.
🤝 Phase 4 – Building Resilience: Strengthening community bonds and promoting positive coping mechanisms.
Result: 75% of participants reported a noticeable improvement in their ability to cope with stress and trauma.
4. Long-Term Support and Community Healing
To ensure the sustainability of the program, additional initiatives were introduced:
✅ Peer-led support networks allowed participants to continue meeting after formal therapy ended.
✅ Referrals to professional mental health services were provided for severe cases.
✅ Economic empowerment programs were integrated, as financial stress was a major contributor to anxiety and depression.
Result: One year after the program, the community saw a 50% reduction in reports of severe psychological distress, and more individuals felt comfortable discussing mental health without stigma.
The Impact: Transforming Lives Through Collective Healing
The introduction of group therapy had profound effects on both individual and community well-being:
📉 PTSD symptoms decreased by 45%, as measured by post-program assessments.
📈 Community cohesion improved, with 80% of participants reporting stronger social connections.
❤️ Participants showed a 60% improvement in emotional resilience, allowing them to regain a sense of purpose.
👥 The program expanded, with participants becoming facilitators for new therapy groups in neighboring villages.
These results demonstrate that mental health support does not always require expensive infrastructure—sometimes, simply bringing people together in a supportive environment can create lasting change.
Conclusion: A Model for Trauma Recovery in Conflict Zones
This case study highlights how group therapy can be a lifeline for individuals living in conflict-affected communities. By fostering shared healing, emotional resilience, and social connection, this initiative proved that mental health recovery is possible, even in the most challenging circumstances.
As conflict continues to affect millions worldwide, similar community-led mental health programs should be scaled and supported. Healing together is not just an idea—it’s a necessity for rebuilding lives and restoring hope.
What’s Next? Expanding the Initiative
To build on this success, the next steps include:
✔️ Training more facilitators to reach underserved areas.
✔️ Securing funding to provide more mental health resources.
✔️ Integrating therapy with vocational training to enhance long-term stability.
This initiative has proven one thing: when people heal together, they rebuild not just themselves but also their communities.