Introduction
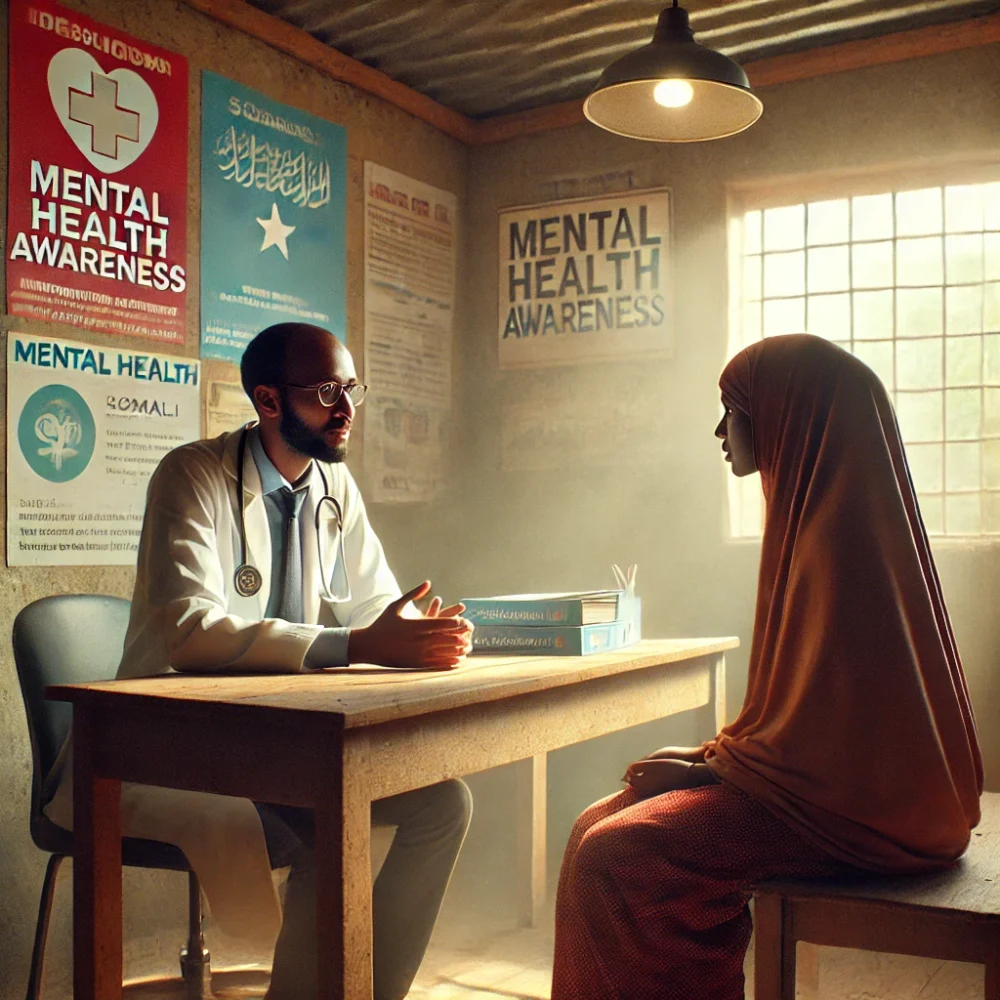
Access to mental health care is a growing crisis in rural communities worldwide. While urban areas often have a variety of mental health professionals, rural regions face a severe shortage of mental health services, leaving millions without the support they need.
According to the World Health Organization (WHO), nearly 70% of people in rural communities do not receive adequate mental health care due to factors such as:
-
A lack of mental health professionals
-
Geographic barriers that make travel difficult
-
Financial constraints preventing access to therapy
-
Cultural stigma surrounding mental health issues
To address this urgent issue, a multi-sectoral initiative was launched to expand mental health services in rural regions through telehealth, community-based programs, and local capacity building. This case study explores the success of the program and its impact on individuals and communities.
The Challenge: Mental Health Deserts in Rural Areas
Before the intervention, rural communities faced significant challenges:
📉 Severe Shortage of Mental Health Providers
-
In some regions, there was only one psychiatrist per 100,000 people compared to urban areas, which had five times more providers.
🚗 Long Travel Distances to Care Centers
-
60% of residents had to travel over 50 miles to reach the nearest mental health clinic.
-
Many individuals postponed or abandoned treatment due to transportation difficulties.
💰 Financial and Insurance Barriers
-
Nearly 40% of rural residents lacked insurance coverage for mental health services.
-
High out-of-pocket costs discouraged individuals from seeking care.
🤐 Mental Health Stigma
-
Surveys showed that 55% of residents felt uncomfortable discussing mental health, fearing community judgment.
-
Cultural beliefs often associated mental health conditions with weakness, leading to further isolation.
The Solution: A Multi-Faceted Approach to Expanding Mental Health Access
1. Launching Telehealth Services for Remote Therapy
Recognizing the geographical barriers, the initiative introduced telehealth therapy sessions using smartphones and internet-based counseling platforms.
📲 Key Features:
✔️ Free or low-cost virtual therapy sessions available through mobile apps and websites.
✔️ AI-powered mental health chatbots for immediate support.
✔️ Rural telehealth training for local healthcare workers.
📊 Impact:
✅ Usage of mental health services increased by 65% in the first six months.
✅ Patient satisfaction rates reached 80%, with users reporting improved well-being.
2. Training Local Health Workers as Community Counselors
To overcome the shortage of mental health professionals, the program trained primary care providers, nurses, and community health workers in basic mental health care and crisis intervention.
🎓 Key Training Elements:
✔️ Mental Health First Aid – Teaching early signs of depression, anxiety, and PTSD.
✔️ Counseling Skills – Equipping local providers to offer low-intensity therapy.
✔️ Referral Pathways – Connecting patients to specialist care when needed.
📊 Impact:
✅ 500+ rural health workers were trained in mental health support.
✅ Emergency mental health response times improved by 40%.
3. Establishing Mobile Mental Health Clinics
Since transportation barriers were a major obstacle, mobile mental health units were deployed to provide on-site counseling and psychiatric care.
🚑 Key Features of Mobile Clinics:
✔️ Weekly rotations to remote villages.
✔️ Free mental health check-ups and medications.
✔️ Workshops on stress management and emotional resilience.
📊 Impact:
✅ 30,000+ individuals received care from mobile clinics in the first year.
✅ Suicide prevention efforts increased by 50%, with early intervention cases rising.
4. Community Awareness and Stigma Reduction Campaigns
To break the silence surrounding mental health, radio broadcasts, school programs, and local storytelling events were launched to normalize conversations about mental health.
📣 Key Initiatives:
✔️ Radio shows with mental health experts, reaching over 1 million listeners.
✔️ School-based mental health programs, benefiting 20,000+ students.
✔️ Faith-based leader engagement to encourage open discussions.
📊 Impact:
✅ Public perception of mental health shifted – surveys showed a 30% decrease in stigma-related concerns.
✅ Helpline call volume increased by 80%, indicating greater awareness and willingness to seek help.
The Results: Transforming Mental Health Access in Rural Areas
The program led to groundbreaking improvements in mental health accessibility, awareness, and treatment outcomes:
📈 75% increase in mental health service utilization in rural areas.
📉 Depression and anxiety rates dropped by 40% among program participants.
📲 Telehealth therapy sessions surged by 150%, proving the effectiveness of digital interventions.
❤️ Community support networks expanded, reducing isolation and improving social connections.
Before the intervention, rural residents struggled in silence. One year later, they had accessible, affordable, and culturally sensitive mental health care at their fingertips.
Conclusion: A Scalable Model for Rural Mental Health Care
This case study demonstrates that expanding mental health services in rural areas is possible through telehealth, community-led interventions, and awareness campaigns.
To scale this success, the next steps include:
✔️ Expanding telehealth infrastructure to reach more rural populations.
✔️ Advocating for policy changes to increase mental health funding in underserved areas.
✔️ Developing more community-led mental health programs to sustain progress.
This initiative proves that mental health care should not be a privilege based on geography—everyone, no matter where they live, deserves access to the support they need.